For many years, the primary focus of stroke prevention has centered on well-known factors like high blood pressure, high cholesterol, and smoking. However, in the field of cardiovascular and sleep medicine, a silent but significant risk factor has gained prominence: Obstructive Sleep Apnea (OSA). The question, can sleep apnea cause stroke, is no longer a matter of debate but a critical area of health investigation. This condition, characterized by repeated pauses in breathing during sleep, can dramatically elevate the risk of a cerebrovascular event. Obstructive sleep apnea is an independent risk factor for stroke, with moderate-to-severe OSA approximately doubling the risk of incident stroke. OSA increases stroke risk, and stroke can cause or worsen OSA.
Understanding the link between sleep apnea and stroke is crucial for early detection and prevention.
This article will explore the physiological mechanisms that connect poor sleep breathing to brain damage, detailing exactly how does sleep apnea cause stroke by damaging the body’s vascular system. It is vital for anyone experiencing symptoms of interrupted sleep to understand this risk, especially given that some individuals are susceptible to having a stroke during their most vulnerable hours—the focus on whether can you have a stroke in your sleep highlights the nocturnal danger posed by OSA.
The Vicious Cycle: How Untreated Sleep Apnea Impacts the Brain and Heart
Obstructive Sleep Apnea (OSA) is far more than just loud snoring. It is a serious medical condition where the upper airway repeatedly collapses, obstructing breathing and causing oxygen levels in the blood to drop (desaturation). These events, which can occur dozens or even hundreds of times per night, trigger a cascade of stressful physiological responses that are devastating to cardiovascular and brain health.
The Mechanics: How Does Sleep Apnea Cause Stroke?
The link between sleep apnea and stroke is a direct result of the body’s frantic attempts to cope with oxygen deprivation. Each time breathing stops, the brain signals a state of emergency, leading to two major issues that directly increase stroke risk:
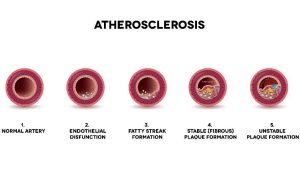
- Surging Blood Pressure: When oxygen levels fall, the body panics, releasing stress hormones like adrenaline. This causes the heart rate to spike and, most critically, leads to powerful, acute surges in blood pressure. These surges are often much higher than daytime blood pressure levels. Over time, these nightly spikes inflict immense damage on the delicate linings of the blood vessels (endothelium), leading to stiffness and the buildup of plaque (atherosclerosis). A stroke—whether ischemic (caused by a clot) or hemorrhagic (caused by a bleed)—is often the end result of these damaged, compromised blood vessels.
- Oxygen Deprivation and Inflammation: The repeated cycles of oxygen desaturation and re-oxygenation create a state of oxidative stress and chronic inflammation throughout the body. Inflammation is a known trigger for clotting, which means the blood is more likely to form blockages. Furthermore, the brain itself is temporarily starved of oxygen during apnea events. If blood flow to the brain is already compromised by damaged arteries, these drops can lead to small, silent strokes over time, or act as a catalyst for a major event. This precisely illustrates how does sleep apnea cause stroke—by generating both the mechanism for clotting and the conditions for blood vessel rupture.
Silent Threat: Can You Have a Stroke in Your Sleep?
Absolutely. Not only can you have a stroke in your sleep, but the period of sleep, particularly during periods of high OSA activity, is a time of heightened risk for a stroke event. Studies have shown a correlation between the time of a stroke and the severity of sleep-disordered breathing. When an apnea event causes a dramatic drop in oxygen and a rapid surge in blood pressure, it creates the perfect storm for a vessel rupture or the dislodgement of a clot.
For those with existing risk factors like hypertension or atrial fibrillation, the nightly strain caused by OSA is particularly perilous. A stroke that occurs nocturnally may go unnoticed for hours, potentially delaying critical medical intervention and leading to more severe long-term disability.
Understanding the Risk: Who is Most Vulnerable to Sleep Apnea and Stroke?
The connection between sleep apnea and stroke is strong across demographics, but certain populations face an especially high risk. Identifying these factors helps target preventative testing and treatment.
- Obesity and Weight: Excess weight, particularly around the neck, is the single greatest risk factor for OSA. This condition, in turn, amplifies the risk of stroke significantly.
- Hypertension (High Blood Pressure): The majority of individuals with OSA also have high blood pressure, making stroke a compounding threat. OSA can make treating high blood pressure much harder, creating a resistant hypertension loop.
- Atrial Fibrillation (AFib): This common heart rhythm disorder substantially increases stroke risk, as it often leads to clot formation in the heart. OSA is a known trigger for AFib, thus linking the two conditions directly to increased stroke incidence.
- Existing Stroke Survivors: Individuals who have already suffered a stroke are at a far higher risk of recurrence. Shockingly, studies show that 40% to 70% of stroke survivors also have OSA, suggesting that untreated sleep apnea may have contributed to the first stroke and threatens to cause the next.
This persistent, profound impact highlights the gravity of the situation and raises the intense public health concern: can you die from a stroke in your sleep? The answer is a clear yes. A catastrophic stroke that occurs during sleep, particularly when the patient is alone and diagnosis/treatment is delayed, carries a higher mortality risk.
Early Detection and Prevention: Taking Control of Your Sleep Health
Given the profound and life-threatening nature of the link—specifically, the potential for can sleep apnea cause stroke—early diagnosis and effective treatment are paramount. Recognizing the symptoms of OSA is the first step toward prevention.
Common Symptoms of Obstructive Sleep Apnea:
- Loud, chronic snoring
- Waking up gasping or choking
- Excessive daytime sleepiness, even after a full night’s rest
- Morning headaches or dry mouth
- Difficulty concentrating, or irritability
When to Seek Help for Obstructive Sleep Apnea (OSA)
If you or a loved one exhibit any of these symptoms, consulting a healthcare professional is non-negotiable. The good news is that diagnosing OSA has become much simpler and more accessible.
Instead of needing a disruptive and potentially expensive night in a hospital lab, many patients are now candidates for a home sleep test. This convenient, user-friendly device allows you to measure your breathing, oxygen saturation, and heart rate from the comfort of your own bed, making the diagnostic process simpler and faster.
Early detection allows for immediate initiation of Continuous Positive Airway Pressure (CPAP) therapy. CPAP is the gold standard of treatment, using a gentle stream of pressurized air to keep the airway open during sleep. By eliminating the breathing pauses, CPAP stabilizes oxygen levels, normalizes blood pressure, and reverses the vascular damage caused by apnea events. This is the single most effective way to mitigate the stroke risk associated with OSA. For those diagnosed with severe OSA, effective treatment often requires a valid CPAP prescription from a physician to start therapy.
Conclusion
The link between Obstructive Sleep Apnea and stroke is undeniable and profound. Untreated OSA subjects the body to nightly cycles of stress that damage blood vessels, elevate blood pressure, and dramatically increase the likelihood of a cerebrovascular event. If you are asking, can sleep apnea cause stroke, the evidence is clear: it is a major and modifiable risk factor. Taking proactive steps to recognize the symptoms and seek diagnosis is perhaps the most important decision you can make for your long-term cardiovascular and brain health. Protect your future by making sure you breathe freely through the night. Start your path to better health today by exploring the option of a convenient, accurate, at-home diagnostic solution.
Take control of your health. Get tested today. If you suspect you have sleep apnea, don’t wait to find out. A simple, physician-approved home sleep test can be shipped directly to your door, offering you the fastest route to diagnosis and life-saving treatment.
Frequently Asked Questions
Does CPAP therapy reduce the risk of stroke?
Yes. Studies consistently show that consistent and compliant use of CPAP therapy significantly reduces blood pressure, oxidative stress, and inflammation—all of which are core risk factors for stroke. For patients with moderate to severe OSA, CPAP acts as a primary preventative measure against cardiovascular events.
Is it true that people often have a stroke in the morning?
While strokes can occur at any time, there is a cluster of events in the early morning hours, often attributed to the natural morning surge of blood pressure. However, for those with severe OSA, stroke risk is significantly elevated during the sleep period itself, particularly when apnea events are at their worst.
Is Obstructive Sleep Apnea worse than Central Sleep Apnea in relation to stroke risk?
Both types increase risk, but Obstructive Sleep Apnea (OSA) is far more common. OSA’s repeated, vigorous efforts to breathe against a blocked airway lead to dramatic, chronic swings in blood pressure and oxygen, making it a powerful and direct driver of stroke risk. Central Sleep Apnea (CSA) involves the brain temporarily failing to signal the need to breathe, and while serious, the mechanism of vascular damage is slightly different.
Sources

Dr. Kunal Agarwal is a highly accomplished board-certified physician specializing in Family Medicine, Sleep Medicine, and Obesity Medicine. He completed his residency at Michigan State University and a fellowship at Henry Ford Health System, and has over a decade of experience delivering exceptional patient outcomes. Dr. Argarwal is passionate about patient education and advocacy, sleep disorders, and more. His expertise in treating sleep apnea is extremely valuable to improve his patients’ lives.
Awards, Honors, & Recognition
Top Doctor
SRQ Magazine and Sarasota Magazine, 2023-2024
Fellow of American Academy of Sleep Medicine (FAASM)
American Academy of Sleep Medicine, 2021
Named “Top Doctor” for 2017, 2018 (on cover), 2019,and 2020 by Delaware Today Magazine
2017-2020