While Obstructive Sleep Apnea (OSA) dominates public discourse regarding sleep disorders, central sleep apnea represents a distinct and often more complex clinical challenge. Unlike OSA, which is characterized by physical airway obstruction, central sleep apnea is a neurological failure where the brain temporarily stops signaling the muscles to breathe. This article explores the pathophysiology of CSA, its diverse etiologies—ranging from heart failure to opioid use—and the specialized therapeutic interventions required to restore respiratory stability.
What is Central Sleep Apnea?
Central Sleep Apnea (CSA) is a sleep-related breathing disorder in which respiratory effort is diminished or absent in an intermittent or cyclical fashion. In a healthy individual, the brain’s autonomic nervous system monitors carbon dioxide (CO2CO_2 ) levels and sends consistent signals to the diaphragm and chest muscles to initiate a breath.
In patients with CSA, this feedback loop is disrupted. The brain “forgets” to breathe, leading to repeated pauses in respiration that result in oxygen desaturation and frequent nocturnal awakenings.
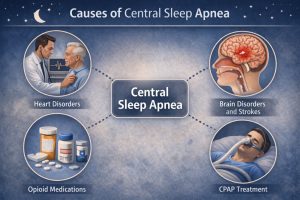
The Diverse Causes of CSA
Understanding what causes central sleep apnea is essential for proper diagnosis and treatment. CSA is rarely a primary condition; it is typically secondary to an underlying medical issue or external factor. The most common central sleep apnea causes include:
Medical Conditions: Congestive heart failure and stroke are primary drivers. In heart failure, a specific pattern called Cheyne-Stokes Respiration often emerges, characterized by a periodic crescendo-decrescendo breathing pattern followed by an apnea. These represent key neurological causes of central sleep apnea that impact the brain’s respiratory control centers.
Drug-Induced CSA: Long-term use of opioid medications can suppress the brain’s respiratory drive, leading to significant central breathing pauses.
High Altitude: At high elevations, lower oxygen levels can trigger “high-altitude periodic breathing” as the body struggles to balance CO2CO_2 and oxygen intake.
Treatment-Emergent CSA: Occasionally, patients being treated for OSA with CPAP develop central apneas once their physical obstruction is cleared—a phenomenon known as Complex Sleep Apnea.
Primary Central Sleep Apnea: In rare cases, idiopathic central sleep apnea occurs without any identifiable underlying cause, though this accounts for a minority of CSA cases. Primary central sleep apnea refers to CSA that is not secondary to another medical condition.
Symptoms and Physiological Effects
Recognizing central sleep apnea symptoms is crucial for early intervention. Because CSA lacks the characteristic “heroic snoring” often found in OSA, it can be much harder to detect. The symptoms of central sleep apnea often present as:
Abrupt Awakenings: Waking up suddenly feeling short of breath or gasping (paroxysmal nocturnal dyspnea).
Excessive Daytime Sleepiness: High levels of fatigue despite a full night’s rest.
Insomnia: Difficulty staying asleep or fear of falling asleep.
Cardiovascular Strain: Repeated oxygen drops put immense pressure on the heart, potentially worsening existing cardiac conditions. These central sleep apnea symptoms warrant immediate medical evaluation.
Therapeutic Approaches and Treatment
Managing CSA requires a highly personalized approach, often starting with treatment for central sleep apnea that addresses the underlying condition (e.g., optimizing heart failure medications). Several central sleep apnea treatments are available:
Positive Airway Pressure (PAP): While standard CPAP is sometimes used, Adaptive Servo-Ventilation (ASV) is often the preferred choice for central sleep apnea treatment. ASV monitors the patient’s breathing in real-time and provides a breath only when the patient’s own respiratory effort fails.
Supplemental Oxygen: Providing extra oxygen can sometimes stabilize the respiratory drive by preventing the “dip” in oxygen that triggers a breathing pause.
Phrenic Nerve Stimulation: For severe cases, an implantable device can be used to stimulate the phrenic nerve, which controls the diaphragm, ensuring a regular breathing rhythm.
The effectiveness of central sleep apnea treatment depends heavily on addressing underlying central sleep apnea causes while simultaneously managing respiratory symptoms.
Final Summation
Central sleep apnea is a sophisticated disorder of the brain-body connection. Its presence is often an indicator of systemic health challenges that require a multidisciplinary approach involving sleep specialists, cardiologists, and neurologists. Early diagnosis is paramount to preventing long-term cardiovascular damage and improving the patient’s quality of life. If you experience gasping during sleep or unexplained exhaustion, seeking a professional evaluation is the first step toward reclaiming your health.
Frequently Asked Questions
1. How is CSA different from OSA?
In OSA, you are trying to breathe but the airway is physically blocked. In CSA, your airway is open, but your body makes no effort to take a breath because the brain hasn’t sent the necessary signal.
2. Can you have both types of sleep apnea at once?
Yes. This is known as “Mixed Sleep Apnea” or “Complex Sleep Apnea.” It usually begins as obstructive but reveals a central component once the physical obstruction is cleared with treatment.
3. Does snoring always mean it’s OSA?
Not necessarily, but snoring is much more common in OSA. CSA patients may not snore at all; their primary symptom is often waking up suddenly feeling like they’ve “forgotten” how to breathe.
4. Is central sleep apnea dangerous?
Yes, both OSA and CSA carry significant risks, but CSA is often associated with more severe underlying illnesses like advanced heart failure or neurological damage, making its clinical management particularly delicate.
5. Is central sleep apnea hereditary?
While CSA itself is not typically inherited, underlying conditions that lead to CSA—such as certain heart conditions or genetic neurological disorders—may have hereditary components. Most cases are acquired rather than inherited.
6. Can I test for CSA with a home sleep test?
Yes. Modern diagnostic technology allows for the detection of central events outside of a laboratory setting. For a convenient and clinical-grade solution, we recommend the Home Sleep Apnea Test from SleepCare Online. Their testing equipment is designed to differentiate between obstructive and central events by accurately measuring respiratory effort.
Ready to understand your sleep? If you or a loved one are experiencing symptoms of gasping or chronic fatigue, a professional diagnosis is essential. Explore your options at www.sleepcareonline.com to get fast, accurate results and a CPAP prescription if required.
Authoritative References
- American Academy of Sleep Medicine (AASM): “The International Classification of Sleep Disorders – Third Edition (ICSD-3).”
- Mayo Clinic: “Central Sleep Apnea: Symptoms and Causes.”
- National Institutes of Health (NIH): “Opioid-Induced Central Sleep Apnea.”