Waking up feeling as though you haven’t slept a wink is a frustrating reality for millions of Americans. Finding the right therapy for sleep apnea is often a journey of trial and error, moving beyond just standard machine-based interventions. While CPAP remains the gold standard for many, a growing number of patients are turning to sleep apnea supportive therapy to bridge the gap in their care or provide comfort during travel. Whether you are struggling with mask leaks or simply looking for a non-invasive supplemental modality, obstructive sleep apnea supportive therapy offers a range of options designed to improve your nightly rest and oxygen saturation. From the targeted use of positional therapy for sleep apnea to the custom-fitted precision of oral appliance therapy for sleep apnea, these adjunct treatments can provide much-needed relief. Before committing to a long-term plan, many individuals begin their journey with an at home sleep apnea test to understand the specific severity of their condition. By combining primary clinical care with the right therapy for sleep apnea, you can finally reclaim your daytime energy and long-term cardiovascular health.
Defining Sleep Apnea Supportive Therapy
When clinicians discuss auxiliary airway management, they are referring to treatments that work alongside or as an alternative to primary ventilation. Sleep apnea supportive therapy is designed to address the specific anatomical or behavioral triggers that cause the airway to collapse during the night. For some, the issue is purely gravitational—the tongue falling back when sleeping on the spine. For others, it is a matter of jaw alignment.
Supportive care is not a “one size fits all” solution. Instead, it is a customized toolkit that helps the body maintain a consistent flow of $O_2$ without necessarily requiring the high pressure of a machine. According to the American Academy of Sleep Medicine, incorporating these supportive measures can significantly increase patient compliance, as they often feel less “medicalized” and more natural than traditional masks.
The Role of Oral Appliance Therapy for Sleep Apnea
For patients with mild to moderate OSA, one of the most effective interventions is a Mandibular Advancement Device (MAD). This form of oral appliance therapy for sleep apnea works by gently shifting the lower jaw forward. This subtle movement creates additional space at the back of the throat, preventing the soft tissues and the tongue from obstructing the passage of air.
Unlike over-the-counter mouthguards, professional appliances are custom-molded to the patient’s unique dental structure. This ensures that the device remains comfortable throughout the night while providing the exact millimetric advancement needed to keep the airway stable. It is a highly portable option, making it a favorite for frequent travelers or those who find CPAP masks too restrictive or claustrophobic.
The Impact of Positional Therapy for Sleep Apnea
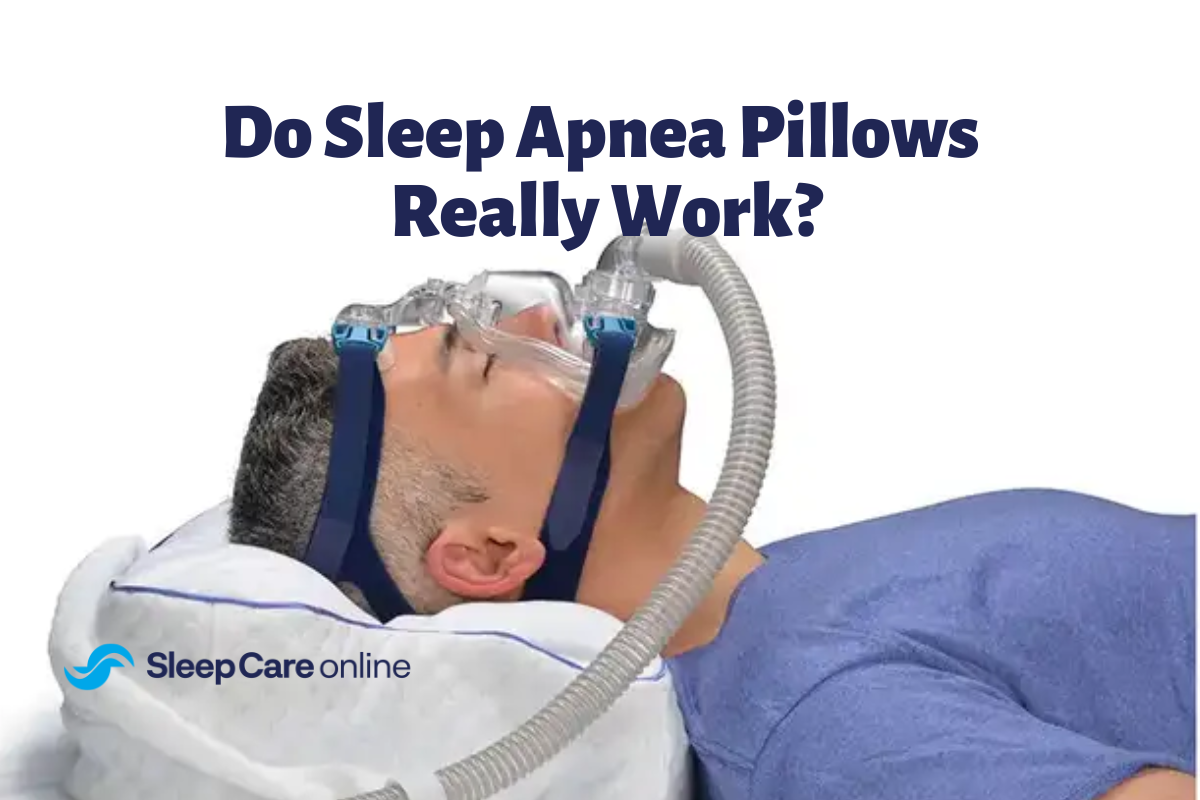
Gravity is a major factor in sleep-disordered breathing. When you sleep on your back (supine), the base of the tongue and the soft palate are more likely to collapse toward the back of the throat. For many, positional therapy for sleep apnea is the simplest and most cost-effective way to reduce the frequency of breathing pauses.
This therapy involves using specialized pillows, wearable sensors, or even simple bumper belts that gently discourage the sleeper from rolling onto their back. Modern positional devices even use gentle vibrations to nudge the sleeper into a side-lying (lateral) position without fully waking them up. By maintaining a side-sleeping posture, the airway remains structurally more open, which can dramatically lower the Apnea-Hypopnea Index (AHI) in positional patients.
Myofunctional Training and Obstructive Sleep Apnea Supportive Therapy
One of the most overlooked aspects of airway stability is muscle tone. Just as we exercise our arms or legs, the muscles of the tongue, soft palate, and throat can be conditioned to remain firm and open. This specialized form of obstructive sleep apnea supportive therapy, often called myofunctional therapy, involves daily “mouth gym” routines.
Incorporating specific exercises for sleep apnea can help tighten the muscles that would otherwise go slack during deep sleep. While these exercises may not replace CPAP for severe cases, they serve as an excellent supportive measure to reduce snoring and improve the overall effectiveness of other treatments. Consistent practice for just 10 to 20 minutes a day can lead to measurable improvements in how the airway responds to pressure changes during the night.
Synergistic Lifestyle Adjustments
Supportive therapy extends beyond devices and exercises; it includes the environment and biological factors we control. Weight management, the avoidance of alcohol before bed, and even humidity control in the bedroom play vital roles. Alcohol, in particular, acts as a potent muscle relaxant, causing the throat tissues to become “floppy” and more prone to collapse.
Furthermore, managing nasal congestion through saline rinses or internal nasal dilators can ensure that the primary intake of air is through the nose rather than the mouth. Mouth breathing is a significant trigger for airway collapse, so any supportive measure that encourages nasal breathing is a win for sleep quality. Combining these lifestyle shifts with mechanical supports creates a comprehensive environment for restorative rest.
Conclusion
Navigating the various options for therapy for sleep apnea can feel overwhelming, but understanding the value of supportive care provides a path toward personalized health. By integrating sleep apnea supportive therapy—whether through positional adjustments, oral appliances, or muscle conditioning—you can create a treatment plan that fits your lifestyle and comfort levels. These interventions are backed by organizations like the Sleep Foundation, proving that a multi-faceted approach to airway management is often the most sustainable. No matter which path you choose, the goal is consistent: to protect your heart, your brain, and your vitality through better oxygenation. Don’t let another night go by in a fog of exhaustion. Take the first step toward a clearer airway and a brighter morning by ordering an at home sleep apnea test today and discovering which treatment path is right for you.
Frequently Asked Questions
What is the difference between primary and supportive therapy?
Primary therapy, like CPAP, is the main tool used to treat the condition. Supportive therapy includes adjunct treatments like positional pillows or oral appliances that help the primary therapy work better or provide an alternative for milder cases.
Can I use positional therapy instead of a CPAP?
This depends entirely on your diagnosis. If your apnea is “position-dependent,” meaning it only happens when you are on your back, positional therapy may be highly effective. However, a doctor must confirm this through a diagnostic study.
Is oral appliance therapy comfortable?
Most patients adapt to a custom-fitted oral appliance within a week. While there may be some initial jaw soreness, the benefit of sleeping without a mask often outweighs the adjustment period.
Do throat exercises really work?
Yes, scientific studies have shown that myofunctional exercises can reduce the severity of OSA by improving the tone of the airway muscles, though they are most effective when used as a supportive measure alongside other treatments.
How do I know which therapy is right for me?
The first step is always a clinical diagnosis. Using an at-home testing kit can provide the data your doctor needs to determine if you require primary mechanical intervention or if you are a candidate for supportive options.